Biocenter Oulu
The main task of Biocenter Oulu is to support high-level research at the University of Oulu and to provide research infrastructure services for the life sciences.
Biocenter Oulu promotes networking of research groups, multidisciplinary approach, as well as cooperation with national and international partners. It organises scientific and collaborative meetings with relevant stakeholders in the field, supports doctoral and post-doctoral researchers and participates in developing doctoral training in collaboration with the University Oulu graduate school.
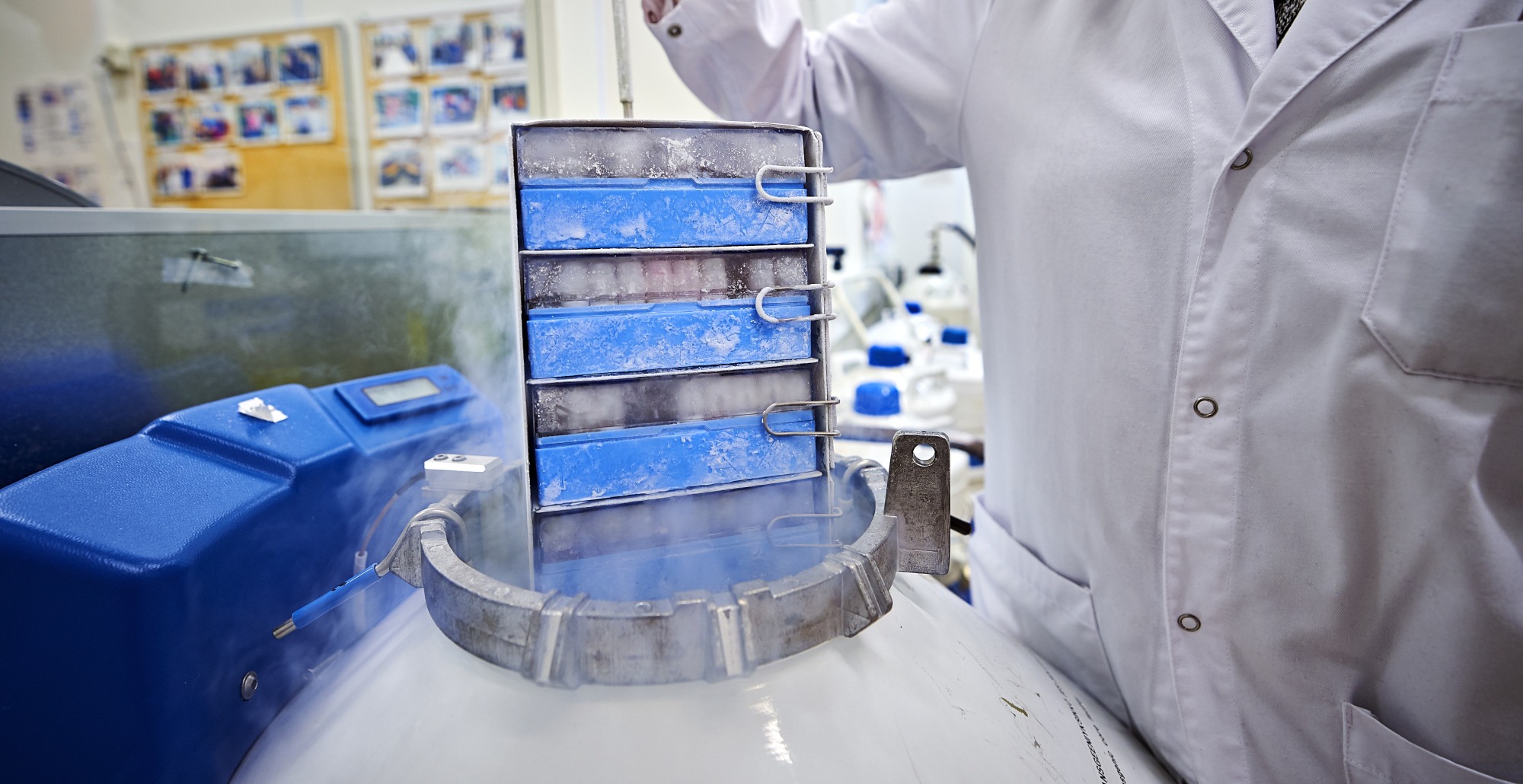
Biocenter Oulu maintains and develops research infrastructure services and provides them with open access principles to support both academic and other customers in their research and R&D projects. These services are part of the nationally distributed Biocenter Finland and the European Research Infrastructure Consortium (EuroBioimaging, Infrafrontier and Instruct ERICs).

The University of Oulu’s strategy strengthens its role as a high-level international science and innovation university that contributes to solving global challenges through the selected focus areas of research. In the Human health and wellbeing research theme the strategic research projects are organized under Biocenter Oulu.
Kontinkangas campus infrastructure for biomedical research
Additional research infrastructure servides provided by the faculties
Biocenter Oulu Data Management Policy
Biocenter Oulu follows University of Oulu general data management policies and regulations and strives to ensure that all data produced by technology platforms will comply with FAIR principles.
Health and Biosciences Doctoral Programme offers field specific doctoral training to its doctoral researchers by organizing courses and other activities and events.
Biocenter Oulu administrative office and majority of the core facilities are located at the Main Building of the Medical Campus, Aapistie 5A, which also houses some of the BCO research groups. The rest of the research groups are situated at the Faculty of Biochemistry and Molecular Medicine, Linnanmaa Campus and at the University Hospital.